Beyond The Skin
Diagnosis
- No clear consensus regarding the diagnostic work-up that should be performed when evaluating patients with AD, particularly adults, has emerged. Diagnostic approaches have large variation.1
- Chronic pruritus and itch induces scratch behavior, which can serve as a physiologic self-protective mechanism to prevent the body from being hurt by harmful external agents, but is well recognized to damage skin and increase inflammation, further exacerbating pruritus, resulting in the ‘‘itch-scratch cycle.’’2
- Clinical phenotypes and endotypes are characterized by a wide range of heterogeneity in the onset, course, and presentation of AD, as well as in individual comorbidities.
- The diagnosis of AD remains clinical. While there is no biomarker to diagnose AD, there are biomarkers that are known to be elevated in disease and can also be used to monitor disease activity including PARC and TIMP-1. 3,4
- Guidelines of care for the management of AD issued in 2023 reported multiple different scales for the measurement of disease severity, without a single gold standard emerging.4
Figure 1: Patient-Related Challenges 11,12
Patient-Related Challenges
- The propensity toward allergic disorders (asthma, food allergy, allergic keratoconjunctivitis, and eosinophilic esophagitis) and skin infection (especially Staphylococcus aureus and widespread herpes/eczema herpeticum) is clearly increased in patients with AD.4 More severe AD appears to have a stronger association with asthma than mild or moderate AD.12
- Neuropsychiatric issues (attention-deficit/hyperactivity disorder, depression, anxiety, conduct disorder, and suicidal ideation) have been recently linked to AD.5
- Assessment of disease severity is further complicated by a disconnect between physicians and their patients. The results of one study suggested that patients and physicians disagreed on the severity level of AD in approximately one-third of cases.6
- Maintaining motivation and treatment adherence in patients with AD is an important, yet often difficult undertaking.
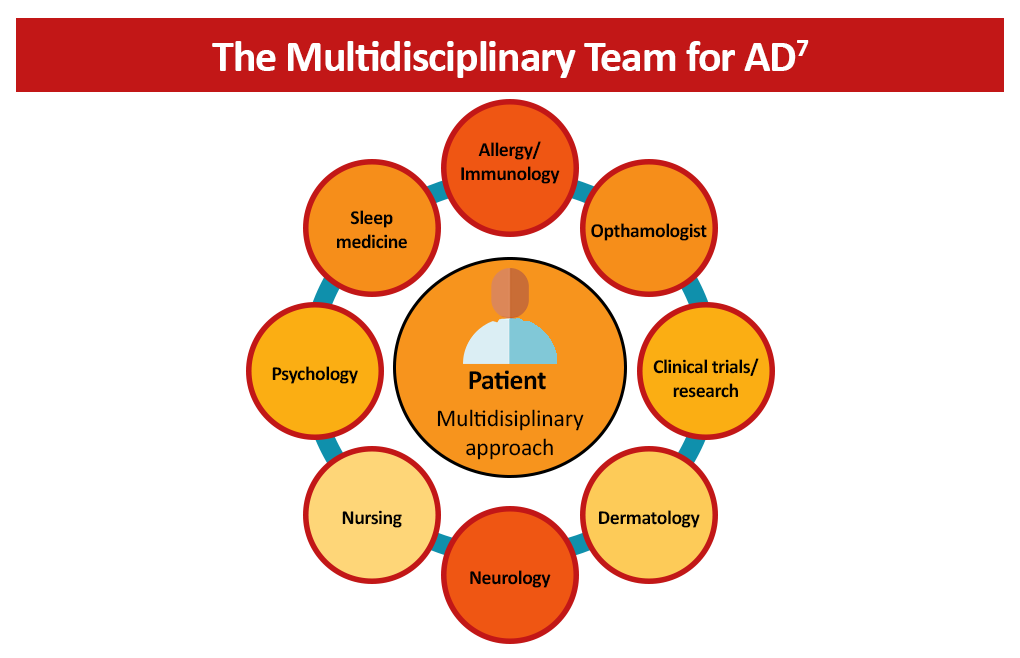
- Proper management of the direct and indirect effects of AD often requires expertise beyond the scope of dermatology. A multidisciplinary approach can treat common comorbidities, improve patient quality of life, reduce polypharmacy, and improve communication between providers.7
Figure 2: The Multidisciplinary Approach to AD 7
References
- Darsow U, Wollenberg A, Simon D, et al. ETFAD/EADV eczema task force 2009 position paper on diagnosis and treatment of atopic dermatitis. J Eur Acad Dermatol Venereol. 2010;24:317-328. https://doi.org/10.1111/j.1468-3083.2009.03415.x
- Paller AS, Kabashima K, Bieber T. Therapeutic pipeline for atopic dermatitis: End of the drought? J Allergy Clin Immunol. 2017;140:633-643. https://doi.org/10.1016/j.jaci.2017.07.006
- Libon F, Caron J, Nikkels A. Biomarkers in atopic dermatitis. Dermatol Ther (Heigelb). 2024;14(7):1729-1738. doi: 10.1007 s13555-024-01193-1
- Chu DK, Schneider L, Asiniwasis RN, et al. Atopid dermatitis (eczema) guidelines: 2023 American Academy of Allergy, Asthma and Immunology Joint Task Force on practice parameters GRADE – and Institute of Medicine-based recommendations. Ann Allergy Asthma Immunol. 2024;132(3):274-312. doi: 10.1016/j.anai.2023.11.009.
- Parisapogu A, Ojinna BT, Choday S, et al. A molecular basis approach of eczema and its link to depression and related neuropsychiatric outcomes: a review. Cureus. 2022;14(12):e32639. doi: 10.7759/cureus.32639.
- Wei W, Anderson P, Gadkari A, et al. Discordance between physician- and patient-reported disease severity in adults with atopic dermatitis: A US cross-sectional survey. Am J Clin Dermatol. 2017;18:825-835. https://doi.org/10.1007/s40257-017-0284-y
- Amerio P, Ferrucci SM, Galluzzo M, et al. A multidisciplinary approach is beneficial in atopic dermatitis. Dermato Ther (Heidelb); 2024:14(6):1443-1455. doi: 10.1007/s13555-024-01185-1.